Search Results for:
Abductor Tendon Repair
Abductor Tendon Tears
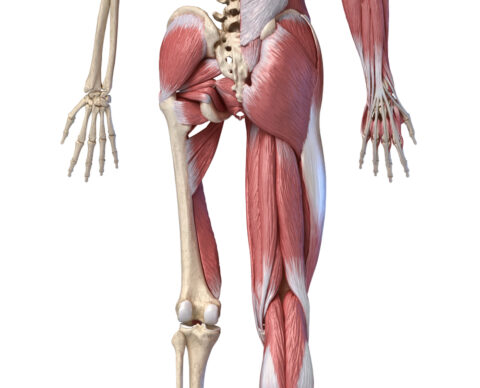
The gluteus medius and minimus muscle tendons work together to stabilize the hip. These tendons are like the rotator cuff of the hip. These tendons insert on the upper portion of the femur at the greater trochanter. Inflammation and/or degeneration of these tendons is called abductor tendonitis. Chronic inflammation of these tendons or trauma to these tendons can result in an abductor tendon tear.
SYMPTOMS & DIAGNOSIS
Patients with abductor tendonitis and/or an abductor tendon tear often present with chronic lateral sided hip region pain. On physical examination, patients are often markedly tender to palpation over the greater trochanter. They may have an abnormal gait called a Trendelenburg gait. A Trendelenburg gait occurs from the weakened abductor muscles and therefore, the pelvis shifts downward to the contralateral side (nonweightbearing side) when walking. The only definitive way to diagnose abductor tendonitis and/or abductor tendon tearing is to order an MRI of the affected hip.
CAUSES OF ABDUCTOR TENDON TEARS
The gluteus medius and minimus tendons can become inflamed and/or tear for a variety of reasons including nicotine use, excess caffeine intake, trauma to the tendons, limited protein intake, use of the antibiotics Ciprofloxacin and/or Levaquin, sleep apnea and frequent cortisone injections into the greater trochanteric bursa. Additionally, hormonal and/or metabolic imbalances such as low vitamin D and hyperparathyroidism can also contribute to abductor tendonitis and/or abductor tendon tearing. We often work up and address any potential causes of the abductor tendonitis/abductor tendon tearing before considering surgical intervention.

TREATMENT OPTIONS
Conservative treatment options for abductor tendonitis include a course of supervised physical therapy, activity modifications, chiropractic care, use of a cane or walking sticks when ambulating to take the pressure off the lateral aspect of the hip and/or anti-inflammatory medications as needed for pain relief. Another treatment option for chronic abductor tendonitis and/or abductor tendon tearing is a platelet-rich plasma injection. Platelet-rich plasma (PRP) injections have been found to be safe and effective in some cases for the treatment of abductor tendonitis and abductor tendon tears. PRP injections are created from the patient’s own blood. Approximately 30-60 cc of blood is drawn from the patient on the day of the procedure. The blood is placed in a centrifuge machine and spun down, which takes approximately 20 minutes. The platelet rich plasma, which is approximately 5-10 cc, is then injected into the abductor tendon to facilitate healing/repair of the damaged tendon. These injections are performed in our office on Friday afternoons. This treatment option is infrequently paid for by insurance companies.
If a course of conservative treatment has been exhausted without substantial improvement in a patient’s symptoms, surgery can be performed to repair the tendon by reattaching it to the bone. The procedure is straightforward, is done as an outpatient surgery and relatively low-risk but the recovery is a long, difficult process. In order for the tendon to heal it needs to be immobilized for two to three months after the surgery in a brace. You are not allowed to put any weight on the operative leg. Often times patients need to go to a rehabilitation center or nursing home for that entire time. The greatest risk of the surgery is that after several months the tendon just doesn’t heal and the symptoms still persist.
Would you like more information? Follow the links below for hand outs and videos regarding Abductor Tendon Repairs
- Abductor Tendonitis – Patient Instructions PDF
- Postoperative Instructions PDF
- Abductor Tendon Repair Physical Therapy Protocol
- How To Wear And Care For A Hip Abductor Brace Video
Here are some helpful images on how to wear the Abductor Brace
About
Orthopedic Doctor Eau Claire
Nathaniel Stewart, MD
Nathaniel Stewart, MD Board-Certified Orthopedic Surgeon Dr. Stewart is an orthopedic surgeon specializing in hip and knee surgery and arthritis procedures in the Eau Claire, Altoona, and Chippewa Falls area. He is the most experienced hip arthroscopist in western Wisconsin and began performing hip arthroscopy in 2000. Being at the forefront of arthroscopic treatment of femoroacetabular impingement, Dr. Stewart has published research in collaboration with the University of Wisconsin – Eau Claire on the relationship between sports participation and femoroacetabular impingement (FAI). Current research includes how FAI can lead to hip arthritis. As a member of the American Association of Hip and Knee Surgeons, Dr. Stewart is dedicated to providing state of the art care for patients with hip and knee joint pain.
Dr. Stewart is an orthopedic surgeon specializing in hip and knee surgery and arthritis procedures in the Eau Claire, Altoona, and Chippewa Falls area. He is the most experienced hip arthroscopist in western Wisconsin and began performing hip arthroscopy in 2000. Being at the forefront of arthroscopic treatment of femoroacetabular impingement, Dr. Stewart has published research in collaboration with the University of Wisconsin – Eau Claire on the relationship between sports participation and femoroacetabular impingement (FAI). Current research includes how FAI can lead to hip arthritis. As a member of the American Association of Hip and Knee Surgeons, Dr. Stewart is dedicated to providing state of the art care for patients with hip and knee joint pain.Learn More
Schedule ![]()
|
Sacred Heart Hospital 900 W. Clairemont Ave. Eau Claire, WI 54701 715.717.4121 (1st, 3rd, 5th) Tuesday AM/PM
|
St. Joseph’s Hospital 2661 Co. Hwy I Chippewa Falls, WI 54729 715.723.1811 (2nd, 4th) Tuesday AM
|
Prevea Rice Lake Health Center 1051 West Avenue Rice Lake, WI 54868 715.719.0662 (2nd, 4th) Tuesday PM
|
CVOSM Chippewa Falls Clinic 757 Lakeland Drive, Ste A Chippewa Falls, WI 54729 715.723.8514 Monday AM
|
|
CVOSM Altoona Clinic 1200 OakLeaf Way, Ste. A Altoona, WI 54720 715.832.1400 Monday PM Wednesday AM/PM |
OakLeaf Surgical Center 1000 OakLeaf Way Altoona, WI 54720 715.831.8130 Thursday AM/PM Friday AM |
Access Patient Information
Advice for Runners with Joint Problems
- Change your running shoes every few months to maintain adequate cushion in your shoes.
- We would encourage you to cross train instead of running multiple days each week. Rotate your exercises between running, biking, elliptical, lifting weights, Pilates and/or yoga. Cross training reduces the amount of time each week that the joints are exposed to high impact loading activities.
- We often encourage our patients to try biking or using an exercise bike instead of running using the Lance Armstrong method to keep their heart rate in the aerobic zone. Lance Armstrong’s method of cycling reduces lactic acid buildup in the muscles by trying to utilize different muscle groups when some fatigue. We encourage you to wear a heart rate monitor while biking to maintain your heart rate in the aerobic zone throughout your workout. As lactic acid starts to build up in your quadriceps, try to recruit other muscles to maintain that target heart rate. You can try “throwing your knees through the handlebars” which recruits your hip flexors. You can try “scraping the gum off your shoes” which recruits your hamstrings and gluteal muscles. You can get up off the seat which recruits your trunk, torso, and arms. By utilizing different muscle groups after some fatigue, it is easier to maintain that target aerobic heart rate which can often give you that “runners high” at the end of your workout.
- You could also try taking glucosamine and chondroitin which are supplements that can be found over the counter. Glucosamine and chondroitin are naturally occurring compounds that are found in the cartilage of joints. Studies have demonstrated modest benefits in arthritic pain by taking these supplements. We would recommend glucosamine sulfate 1,500 mg and chondroitin sulfate 1,200 mg daily.
Ajax Search Results
Bilateral Total Hip Arthroplasty
What is Bilateral Total Hip Arthroplasty?
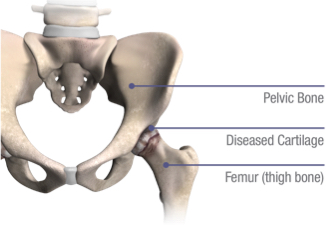
Bilateral total hip arthroplasty is a procedure in which both diseased hips are replaced. Dr. Stewart began performing bilateral total hip arthroplasties in 2015 for patients with severe osteoarthritis in both hips. Bilateral total hip arthroplasties allow patients to reduce the length of recovery in comparison to undergoing two consecutive hip replacements, which would need to be spaced out at least 6-12 weeks apart.
PAIN POINTS
What is Degenerative Joint Disease (DJD)?
Degenerative joint diseases (DJDs) are chronic conditions often resulting in pain and the loss of an active lifestyle and quality of life.
There are different types of DJD that can affect the hip, including:
- Osteoarthritis (OA), in which cartilage wears down over time
- Post-traumatic arthritis, which results from a severe fracture or dislocation of the hip
- Rheumatoid arthritis (RA), an inflammatory arthritis of the joints
- Avascular necrosis (AVN), a condition where the ball or femoral head of the hip joint has lost a healthy supply of blood flow causing the bone to die and the femoral head becomes misshaped
- Hip dysplasia, a condition where bones around the hip joint did not form properly, which may cause misalignment of the hip joint
THE CAUSE
What Causes Degenerative Joint Disease?
The risk of developing symptomatic, degenerative joint disease is influenced by multiple factors such as age, gender and inherited traits that can affect the shape and stability of your joints. Other factors can include:
- A previous hip injury
- Repetitive strain on the hip
- Improper joint alignment
- Being overweight
- Exercise or sports-generated stress placed on the hip joint

BILATERAL TOTAL HIP ARTHROPLASTY
Risks/Benefits of Bilateral Total Hip Arthroplasty:
There is a slight increased risk of requiring a blood transfusion when undergoing bilateral total hip arthroplasties, however, the risk is still quite small. Our patients who have undergone bilateral total hip arthroplasties have done exceptionally well and have had a very similar postoperative recovery to those patients that have undergone a single hip replacement.
Bilateral Total Hip Arthroplasty
Patients who have severe osteoarthritis of the bilateral hips and are in good physical health are good candidates for bilateral total hip arthroplasty. Ideal surgical candidates for bilateral total hip arthroplasty are those who are less than 65 years old, non-smokers, have a BMI less than 40 and are relatively healthy with few or no medical comorbidities.
The benefits of undergoing bilateral total hip arthroplasty versus staged hip replacements include not being exposed to anesthesia twice and less time off work to recover. There are minimal additional risks associated with undergoing bilateral total hip arthroplasty vs a single hip replacement. There is a slightly increased risk of needing a blood transfusion. In our initial experience, only two of our patients who underwent bilateral total hip arthroplasty required a blood transfusion postoperatively. Patients who undergo bilateral total hip arthroplasty have a very similar recovery to someone who undergoes a single hip replacement. The majority of our bilateral total hip arthroplasty patients are discharged home the day after surgery.
If you have questions regarding bilateral total hip arthroplasty, we would be happy to see you in our clinic or discuss any questions you may have over the phone. You can call our office to schedule an appointment to see Dr. Stewart and/or reach us to discuss questions over the phone at (715) 832-1400.
Blog
Case Study – Bilateral Total Hip Arthroplasty
Cynthia is a very pleasant 65-year-old female patient of Dr. Stewart’s who underwent bilateral total hip arthroplasty in November of 2015.

ABOUT CYNTHIA
Cynthia had severe osteoarthritis in both of her hips, which was significantly impacting the quality of her life.
Prior to surgery, she had difficulty walking, bending over, going up and down the stairs, and carrying items due to arthritis pain in her hips. She made the decision to pursue bilateral total hip arthroplasty to relieve her discomfort and to improve her quality of life.
HOW DR. STEWART HELPED
She had a very good experience having her hip surgery performed at Sacred Heart Hospital.
Cynthia was very diligent about participating in physical therapy and performing her exercises on her own at home. She states she was able to return to activities of daily living approximately 2-3 weeks after her hip surgery and she had returned to working full time within 6 weeks of her surgery. She felt that she was fully recovered by 4 months postoperatively.


THE RESULT
Cynthia is very pleased with the outcome of her surgery.
Cynthia is very pleased with the outcome of her orthopedic surgery. She can now do all of the things she could not do preoperatively with hip arthritis including walking, bending over, going up and down the stairs and carrying items without any hip pain.