Posted on January 9, 2017 by Josh -
Kim is a very active patient of Dr. Stewart’s and the head volleyball coach at UW Eau Claire who underwent a bilateral hip arthroscopy, one during 2012 and the other during 2013.
ABOUT KIM
Kim had femoracetabular impingement which subsequently lead to labral tears in both of her hips causing substantial discomfort. (Read about hip pain injury symptoms here.)
Prior to undergoing her hip arthroscopy, she had difficulty and pain when playing with her daughter on the floor and lifting her in and out of the car seat. She made the decision to undergo a bilateral hip arthroscopy to reduce her discomfort and improve her quality of life.
HOW DR. STEWART HELPED
Kim is very satisfied with the result of her surgeries and is still doing excellent several years after having undergone hip arthroscopy
Within a few months of undergoing her hip arthroscopy, she returned to a very active lifestyle being the head volleyball coach at UW Eau Claire. She was able to hit volleyballs at her players, move around on the volleyball court, stand for prolonged periods of time both in volleyball camps and during matches without any pain. Prior to her surgeries, these activities would cause significant pain and her pain would last for several days in duration. She states within six months of undergoing her hip arthroscopy she could play volleyball at full strength.


THE RESULT
Kim had an excellent experience having her hip arthroscopy performed at Oakleaf Surgical Hospital.
She was surprised by how quickly her pain resolved following her surgery. She states that as soon as she had surgery, she noticed immediate relief of the low back and pelvic pain she was experiencing preoperatively. “To be able to go back and be as active as I am both in coaching and also with my family and little children has been really awesome to be pain free again.”
Posted on January 9, 2017 by Josh -
Orthopedic Surgery Preparation
Following these preparation steps will allow the procedure and healing process to run as smooth as possible.
Preparing for Orthopedic Surgery
Patient Information
If you are having Day Surgery, remember the following:
- Have someone available to take you home, you will not be able to drive for at least 24 hours.
- Do not drink or eat anything in the car on the trip home.
- The combination of anesthesia, food, and car motion can quite often cause nausea or vomiting. After arriving home, wait until you are hungry before trying to eat. Begin with a light meal and try to avoid greasy food for the first 24 hours.
- If you had surgery on an extremity (leg, knee, hand or elbow), keep that extremity elevated and use ice as directed. This will help decrease swelling and pain.
- Take your pain medicine as directed. Begin the pain medicine as you start getting uncomfortable, but before you are in severe pain. If you wait to take your pain medication until the pain is severe, you will have more difficulty controlling the pain.
Posted on January 9, 2017 by Josh -
Total Hip Arthroplasty: What is Direct Anterior Approach Hip Replacement Surgery?
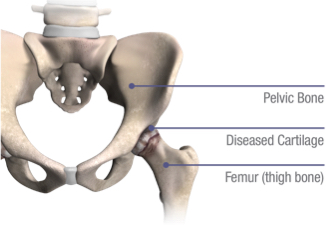
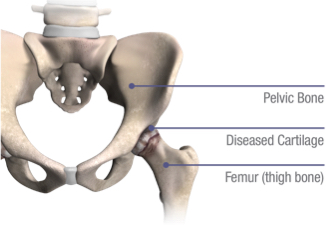
Total hip arthroplasty is a surgical procedure in which cartilage and bone that were damaged by arthritis are removed from the hip joint and replaced with artificial joint components. This can help relieve hip joint pain from arthritis and restore the normal alignment and function of your hip. In December of 2013, Dr. Stewart transitioned to using the direct anterior approach for hip replacement surgery. He now performs greater than 99% of his hip replacements through this method. The direct anterior approach hip replacement is becoming an increasingly popular method for performing total joint replacement surgery due to the numerous benefits it provides. The approach is the method an orthopedic surgeon uses to get to the hip joint for hip replacement surgery. The direct anterior approach is a surgical technique that allows the orthopedic surgeon to access the joint where the hip pain is on the anterior surface, which is diagrammed below.
PAIN POINTS & Arthritis
What is Degenerative Joint Disease (DJD)?
Degenerative joint diseases (DJDs) are chronic conditions, often resulting in hip pain and the loss of an active lifestyle and quality of life. DJDs may result in a person needing hip replacement.
There are different types of DJD that can affect the hip, including:
- Osteoarthritis (OA), in which cartilage wears down over time
- Post-traumatic arthritis, which results from a severe fracture or dislocation of the hip
- Rheumatoid arthritis (RA), an inflammatory arthritis of the joints
- Avascular necrosis (AVN), a condition where the ball or femoral head of the hip joint has lost a healthy supply of blood flow causing the bone to die and the femoral head becomes misshaped
- Hip dysplasia, a condition where bones around the hip joint did not form properly, which may cause joint misalignment and hip pain
THE CAUSE
What Causes Degenerative Joint Disease?
The risk of developing symptomatic, degenerative joint disease, or arthritis, is influenced by multiple factors such as age, gender, and inherited traits that can affect the shape and stability of your joints. Other factors that can contribute to hip pain and joint disease include:
- A previous hip injury causing arthritis
- Repetitive strain on the hip
- Improper joint alignment
- Being overweight
- Exercise or sports-generated stress placed on the hip joint

TREATMENT
Benefits of the Direct Anterior Approach Hip Replacement Surgery Include:
- Less muscle damage and hip pain
- Faster recovery
- Reduced risk of hip dislocation
- More accurate component positioning
- Fewer restrictions
Recovery from Direct Anterior Approach Hip Replacement Surgery:
Most patients who undergo direct anterior approach hip replacement surgery are able to bear weight as tolerated on the surgical leg immediately after surgery. Dr. Stewart may put you on a weight-bearing restriction for a few weeks to reduce your risk of developing a stress fracture, however, this is quite rare. The nursing staff and physical therapists will assist you with walking shortly after hip surgery. Most of our patients use a walker for the first 1-2 weeks and then gradually transition to a cane, and eventually to no-gait aids. Generally, patients who undergo direct anterior total hip joint replacement surgery stay in the hospital one night and then go home the next day. We will arrange for you to undergo outpatient physical therapy 1-2 times per week for the first 3-4 weeks after surgery. We put all of our patients on a blood thinner postoperatively to reduce the risk of developing a blood clot. You will have a postoperative follow-up appointment with Dr. Stewart 10-14 days after your direct anterior approach surgery. Orthopedic Surgeon, Dr. Stewart, serves patients in the Altoona, Eau Claire, and Chippewa Falls area and is ready to talk with you today.
For more detailed postoperative recovery instructions, please see our patient resources page.
Learn More
Posted on January 9, 2017 by Josh -
 Provided below are documents to help with the process of the procedures including Pre-op outline, Pre-op letters to provide to primary care providers and an AUASS scoring sheet. Feel free to contact us with any other questions regarding orthopedic doctor resources.
Provided below are documents to help with the process of the procedures including Pre-op outline, Pre-op letters to provide to primary care providers and an AUASS scoring sheet. Feel free to contact us with any other questions regarding orthopedic doctor resources.
Documents to Help with Orthopedic Doctor Procedures
Download these forms to fill out below:
 Pre-op PT Outline
Pre-op PT Outline
 Letter to PCP for HP
Letter to PCP for HP
 AUASS Score
AUASS Score
 DVT Prophylaxis Protocol
DVT Prophylaxis Protocol
Posted on November 7, 2017 by Josh -
Postoperative complications occur in approximately 2% of individuals that undergo total joint arthroplasty. One of the most common surgical complications following total joint arthroplasty is a deep venous thrombosis (DVT), or more commonly referred to as a blood clot. We strive to reduce the risk of our patients from developing a blood clot by treating them prophylactically with an anticoagulant postoperatively. The two main forms of anticoagulation we use are aspirin and Coumadin. We have a list of criteria that we use to help determine which patients are at a higher risk of developing a blood clot and those individuals are treated with Coumadin for three weeks postoperatively. Patients who are at a lower risk of developing a blood clot are put on aspirin for one month postoperatively. Some of the risk factors that increase an individuals chance of developing a blood clot include age over 70, BMI greater than 40, personal or family history of a blood clot, certain clotting disorders and the use of birth control pills or hormone replacement therapy. For a more comprehensive list of risk factors, please download our DVT Prophylaxis Protocol which is provided in a PDF format below.
 DVT Prophylaxis Protocol
DVT Prophylaxis Protocol
Posted on August 26, 2021 by Summer -
Hip Arthroscopy, Rotational Osteotomies & Abductor Repairs
Posted on January 9, 2017 by Josh -
GENERAL QUESTIONS
HIP REPLACEMENT QUESTIONS
- What is a hip replacement?
Hip replacement involves the removal of arthritic bone ends and damaged cartilage and replaces them with prosthetic implants that replicate the hip joint. Hip replacement can help relieve pain and get you back to enjoying normal, everyday activities.
- What are the reasons for total hip replacement?
Total hip replacement is often reserved for patients who have a painful, disabling joint disease of the hip resulting from a severe form of arthritis.
- How is a total hip replacement performed?
In a total hip replacement operation, the surgeon replaces the worn surfaces of the hip joint with an artificial hip joint. The worn head of the femur (thighbone) is replaced with a ceramic ball mounted on a stem; the stem is placed firmly into the canal of the thighbone at its upper end. The acetabulum (hip socket) is prepared and implanted with a metal cup and plastic insert. The ceramic ball and plastic insert glide together to replicate the hip joint. Dr. Stewart transitioned to using the direct anterior approach in December of 2013. He performs the vast majority of his primary total hip replacements using the direct anterior approach.
- How do I know if I am a candidate to have my hip replacement performed through the direct anterior approach?
Dr. Stewart performs greater than 99% of his primary total hip replacements through the direct anterior approach. There are very few instances when the direct anterior approach cannot be performed.
- Who should have a hip replacement?
Hip replacement surgery may be considered when arthritis limits your everyday activities such as walking and bending, when pain continues while resting, or stiffness in your hip limits your ability to move or lift your leg. Hip replacement may be recommended only after careful diagnosis of your joint problem. It may be time to consider surgery if you have little pain relief from anti-inflammatory medications and intra-articular cortisone injections or if other treatments, such as physical therapy, do not relieve hip pain.
- How long is the hospital stay?
After hip replacement surgery, the majority of our patients are discharged on postoperative day one. Our patients typically ambulate with a walker within a few hours of their surgical procedure. The vast majority of our patients are able to bear weight as tolerated on the surgical leg. In rare instances, Dr. Stewart has patients limit the amount of weight they are able to bear on their surgical side depending on the quality of the bone. This will be addressed with you postoperatively if he identifies that you have poor bone quality during the surgery. We also recently began the fast track recovery program at Oakleaf Surgical Hospital where select patients have the option of being discharged home the day of their surgery if they feel up to it.
- How long is recuperation?
Recovery varies for each individual patient. It is essential that you follow your orthopedic surgeon’s instructions regarding home care during the first few weeks after surgery; especially concerning the exercise program you are prescribed. You should be able to resume most normal light activities of daily living within three to six weeks following surgery. Some discomfort during activity and at night is common for several weeks. Complete recovery can take from about three to six months.
While most people will gradually increase their activities and return to doing things like playing golf, doubles tennis, shuffleboard, or bowling, you will be advised to avoid more active sports, such as jogging, singles tennis, and other high-impact activities.
- Could there be complications?
As with any surgery, there is a risk of complications after hip replacement surgery. However, they are relatively rare. Blood clots are the most common complication after surgery. You will be started on Xarelto postoperatively to help prevent the development of a blood clot. You will also be asked to wear TED stockings, which are compression type stockings, for the first three weeks postoperatively to reduce the risk of developing a blood clot.
- What is the success rate?
Hip replacement is one of the most important surgical advances of this century. This surgery helps more than 300,000 Americans each year to relieve their pain, and get back to enjoying normal, everyday activities.
- How long does a hip replacement last?
Dr. Stewart has been using the Stryker Accolade II stem and the trititanium acetabular cup and/or the PSL acetabular cup for several years now depending on the size of implant needed. These implants have been used for the past decade and have a 10-year success rate of 97%.
- When can I discontinue dressing changes?
Generally, dressings should be worn for the first few days following the surgery. However, if there is no longer any drainage from the incision, dressing changes may be discontinued.
- How long should I wear the TED stockings after undergoing total hip arthroplasty?
We recommend that you wear your TED stockings for the first three weeks following your surgery to reduce the risk of developing a blood clot.
- How long will I be on a blood thinner postoperatively?
All of our patients who undergo joint replacement are placed on a blood thinner for the first three weeks postoperatively. Depending on your personal and family history and recovery process, you may be stopped as early as two weeks postoperatively.
BIRMINGHAM HIP RESURFACING
- Since the BIRMINGHAM HIP* Resurfacing implant is new in the United States, is it clinically proven?
While the BIRMINGHAM HIP* Resurfacing implant is new to the United States, it is not a new implant or technique. It has been in use worldwide since 1997, and the US Food and Drug Administration reviewed a tremendous amount of resulting clinical data before approving it for use in this country.
- Who is a candidate for the BIRMINGHAM HIP* Resurfacing System?
The typical patient will be physically active, under 60 years of age, and suffering from hip arthritis, hip dysplasia or avascular necrosis of the hip. The implant can be used in patients over 60 whose bone quality is strong enough to support the implant. Your surgeon will make the determination if you are a candidate for hip resurfacing.
- How long will the BIRMINGHAM HIP* Resurfacing implant last?
It is impossible to say how long your implant will last because so many factors play into the lifespan of an implant. A clinical study showed the BIRMINGHAM HIP* Resurfacing implant had a survivorship of 98.4-percent at the five-year mark.
- How long will my scar be?
Your surgeon will use an incision of between six and eight inches in length. While some surgeons may use a slightly smaller incision, most will fall in that range.
- What are my physical limitations after surgery?
Most surgeons will tell you that after the first year, you can return to whatever physical activity you enjoyed before hip pain limited your mobility. For instance, unlike total hip replacement, you will be able to return to jogging or singles tennis after your first year after surgery. During your first year, more conservative, low-impact activities like walking, swimming and bicycling are recommended for strengthening your femoral neck and the muscles around your resurfaced joint.
- How can I receive more information about hip resurfacing and the BIRMINGHAM HIP* implant?
KNEE REPLACEMENT
- What is knee replacement?
Knee joint replacement is a surgical procedure in which certain parts of an arthritic or damaged knee joint are removed and replaced with a prosthesis, or artificial joint. The artificial joint is designed to move just like a normal, healthy joint and allows you to get back to enjoying normal, everyday activities without pain.
- How bad does my joint pain have to get before I should consider having joint replacement?
This is a very personal decision that only you can make with the help of an orthopedic specialist’s evaluation of your pain and its effects on your daily life. For example, experiencing knee pain day after day without relief can lead to “staying off” the joint. This often weakens the muscles around it, so it becomes even more difficult to move.
When other more conservative treatment options, including medication and physical therapy, no longer provide pain relief, joint replacement may be recommended.
- What will I need to know about postoperative recovery in the hospital?
Following joint replacement surgery, hospital stays vary depending on insurance coverage and individual medical status. The majority of our patients remain in the hospital for 1-2 days following their knee replacement. Our patients ambulate with the assistance of a walker within hours of their surgery. A physical therapist will work with you while you are in the hospital to get you moving following your knee replacement surgery. The majority of our patients are discharged to home if they have an able bodied person to assist with their recovery process. However, we do have some patients that are discharged to a rehabilitation facility for a short time to assist with their recovery process if they do not have somebody that can help them at home.
-
What can I expect in the first days after I'm discharged?
You shouldn’t be surprised if you feel a little shaky and uncertain for the first day or two after you’re discharged. But soon you may get a routine going and gain confidence in your new joint — the start of a new life with less pain. As with any surgery, you’ll probably take pain medication for a few days while you are healing. Be aware that you’ll probably need a walker and/or crutches for 2-3 weeks following your surgery and then transition to a cane or no-gait aid depending on the recovery process.
-
When will I be able to go back to a normal daily routine, such as going to work or driving a car?
We recommend that patients take 4-6 weeks off work if they have a light duty job where they spend the majority of their day sitting. If someone has a heavy duty job such as construction work or a job that requires them to be on their feet most of the day, we recommend taking 8-10 weeks off work. Most of our patients are able to resume driving within 1-2 weeks after surgery as long as they have discontinued narcotic pain medication and they feel strong and alert enough to drive.
- How long does a knee replacement last?
As successful as most of these procedures are, over the years the artificial joint can become loose or wear out, requiring a revision (repeat) surgery. How long it will last depends not only on a person’s age, but also on a patient’s activity level. These issues, together with the fact that increasing numbers of younger and more active people are receiving total joint replacement, have challenged the orthopedic industry to try to extend the life cycle of total joint replacements.
- What happens during knee replacement surgery?
In surgery, the knee is flexed and the leg suspended. One muscle is separated to expose the femur (thighbone); later, the tibia (shinbone) is exposed. The damaged surfaces at the end of the thighbone are trimmed and shaped to fit inside the total knee prosthesis. The shinbone is cut flat across the top and a hole is created in the center to hold the stem of the tibial component. If needed, the knee cap is trimmed and the patellar component attached.
At various points during surgery, the alignment, function, and stability of the knee joint are evaluated and required adjustments are made. The prosthesis components are cemented into place, any contracted ligaments are released, the midvastus muscle is reconstructed, and the incision is closed.
- When can I discontinue dressing changes?
Generally, dressings should be worn for the first few days following the surgery. However, if there is no longer any drainage from the incision, dressing changes may be discontinued.
- How long will I be on a blood thinner postoperatively?
All of our patients who undergo joint replacement are placed on a blood thinner for the first three weeks postoperatively. Depending on your personal and family history and recovery process, you may be stopped as early as two weeks postoperatively.
Posted on January 9, 2017 by Josh -
Posted on January 9, 2017 by Josh -
SYMPTOMS
Common symptoms relating to hip pain injuries and problems
Many of our patients in Eau Claire and Altoona come to our office for evaluation of a specific symptom related to hip pain. It is our responsibility and privilege to obtain an accurate history, physical examination and obtain any necessary imaging studies, including x-rays and/or MRI, to determine a diagnosis for those symptoms. We then collaborate with our patients to create an individualized hip pain treatment plan that meets each of their needs. Listed below are several hip symptoms we often see patients for in our clinic:
- Groin pain
- Hip pain
- Buttock pain
- Knee pain
- Thigh pain
- Instability
- Catching
DIAGNOSES
Common conditions that we treat.
There are also instances when patients will be referred to our office by another practitioner seeking treatment for a specific condition.
Below is a list of conditions we commonly treat:
- Osteoarthritis of the hip
- Avascular necrosis of the hip
- Transient osteoporosis
- Femoracetabular impingement
- Labral tear
- Failed hip replacement
- Infected hip replacement
- Hip fractures
- Abductor tendonitis and/or tears
- Ischial tendonitis
Posted on January 9, 2017 by Josh -
What is Hip Arthroscopy?
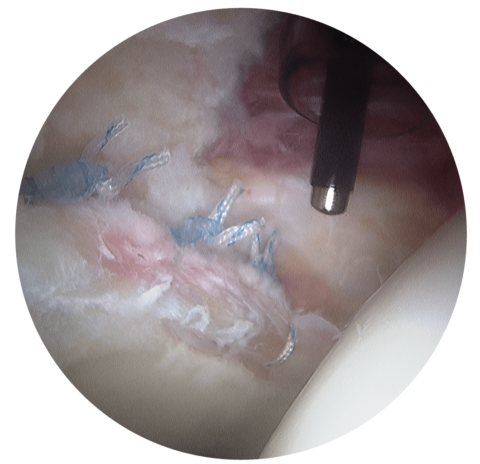
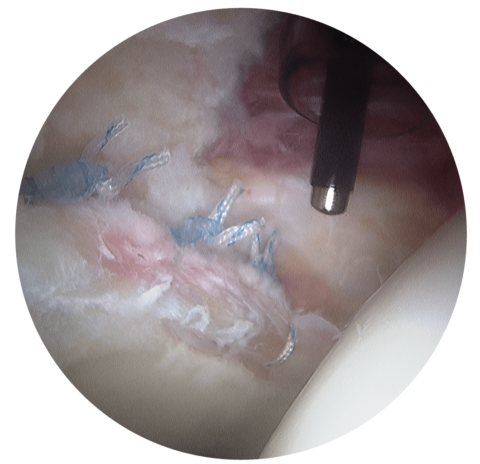
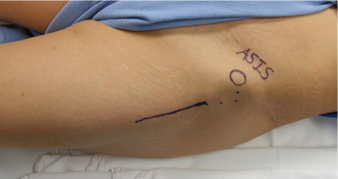
Hip arthroscopy is a minimally invasive surgery that is performed through 2-3 very small incisions to evaluate and treat a variety of hip conditions. During a hip arthroscopy, Dr. Stewart inserts a small camera through one of the incision sites that then provides an image up on a screen for him to view the hip joint. He then places small surgical instruments through the incision sites to correct the hip pathology that is present and causing your symptoms.

PAIN POINTS & ARTHRITIS
Hip arthroscopy may be indicated for the following reasons:
- Debridement of loose bodies: Bone chips or torn cartilage debris cause hip pain and decreased range of motion and can be removed with hip arthroscopy.
- Femoroacetabular impingement: Femoroacetabular impingement, or FAI, is a condition resulting from abnormal pressure and friction between the ball and socket of the hip joint resulting in pain and progressive hip dysfunction. When left untreated, this leads to the development of secondary osteoarthritis of the hip and may require an arthritis doctor.
- Removal of adhesions: Adhesions are areas of built up scar tissue that can limit movement and cause pain.
- Snapping iliopsoas tendon: When the iliopsoas tendon rubs over the front of the hip joint, some patients experience discomfort, particularly with hip flexion. This tendon can be surgically released through hip arthroscopy to eliminate the rubbing over the front of the hip joint.
- Repair of torn labrum: The labrum lines the outer edge of the “socket,” or acetabulum, to ensure a good fit. Tears can occur in the labrum causing hip pain.
- Removal of bone spurs: Extra bone growth caused by injury or arthritis that damages the ends of the bones cause pain and limited joint mobility.
- Partial Synovectomy: Removal of portions of the inflamed synovium (joint lining) in patients with inflammatory arthritis can help to decrease the patient’s pain. However, a complete synovectomy requires an open, larger hip incision.
- Debridement of joint surfaces: Conditions such as arthritis can cause the breakdown of tissue or bone in the joint.
- Repair after Trauma: Repair of fractures or torn ligaments caused by trauma.
- Evaluation and diagnosis: Patients with unexplained pain, swelling, stiffness and instability in the hip that is unresponsive to conservative treatment may undergo hip arthroscopy for evaluation and diagnosis of their condition.
ARTHROSCOPY: WHAT TO EXPECT
What imaging studies are ordered if you are to undergo hip arthroscopy?
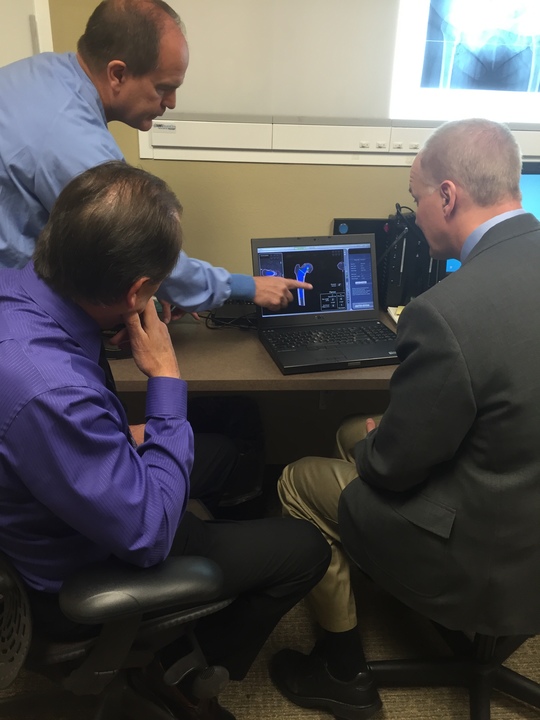
At your first office visit to see Dr. Stewart, we always obtain an x-ray of the hip to evaluate for any evidence of femoracetabular impingement, osteoarthritis, hips dysplasia or other pathologic causes for hip pain. If you are a candidate for hip arthroscopy, we generally need to obtain an MRI of the hip as well as a 3D CT scan of your hip for surgical planning purposes. These studies are not ordered until after you see Dr. Stewart and feel strongly about pursuing surgical intervention for your hip pain. In some instances, if a patient has degeneration of the hip joint and early to moderate osteoarthritis they may not be considered a candidate for hip arthroscopy.
Risks of hip arthroscopy:
The risks of hip arthroscopy include potential risk of blood clot, infection, injury to an artery or nerve, adverse reaction to the anesthetic and the possibility that hip arthroscopy will not adequately alleviate symptoms.

HIP ARTHROSCOPY SURGERY
About Hip Arthroscopy Surgery:
Hip arthroscopy is an outpatient procedure, so you will go home the same day as your surgery. You will need someone to drive you home from the surgery and will likely need help for the first 1-2 days after surgery. Our patients begin outpatient physical therapy the day after their surgery and we recommend going to therapy 2-3 times per week for several weeks following the hip arthroscopy. All of our patients take naproxen twice daily after surgery to reduce the risk of excess bone growth at the surgical site, called heterotopic ossification. We also put patients on aspirin to prevent the risk of developing a blood clot. Generally, our patients use crutches for the first few weeks after surgery. Depending on hip pathology present and procedure performed, some patients are able to bear weight immediately following the surgery, however, others are expected to be 20% weight bearing for the first two weeks post-op. You will be instructed on any weight bearing restrictions prior to being discharged from the hospital
If you have questions about hip arthroscopy in the Eau Claire, Altoona and Chippewa Falls area, contact Dr. Stewart today.
To learn more about Hip Arthroscopy, view some of the links below:
- Kuhns, B. D., Weber, A. E., Levy, D. M., & Wuerz, T. H. (2015). The Natural History of Femoroacetabular Impingement. Frontiers in Surgery, 2, 58. http://doi.org/10.3389/fsurg.2015.00058
- Siebenrock, K. A., Ferner, F., Noble, P. C., Santore, R. F., Werlen, S., & Mamisch, T. C. (2011). The Cam-type Deformity of the Proximal Femur Arises in Childhood in Response to Vigorous Sporting Activity. Clinical Orthopedics and Related Research, 469(11), 3229–3240. http://doi.org/10.1007/s11999-011-1945-4
- Tibor, L. M., & Leunig, M. (2012). The pathoanatomy and arthroscopic management of femoroacetabular impingement. Bone & Joint Research, 1(10), 245–257. http://doi.org/10.1302/2046-3758.110.2000105
- Beck, M., Kalhor, M., Leunig, M., & Ganz, R. (2005). Hip morphology influences the pattern of damage to the acetabular cartilage. Bone & Joint Journal, 87-B(7), 1012-1018. Accessed January 11,
2017. https://doi.org/10.1302/0301-620X.87B7.15203.
- Stewart, N.J. (2007). Oakleaf Surgical Hospital’s Healthy Viewpoints. Accessed January 11, 2017. http://www.oakleafsurgical.com/hv/2007_win/win2007_hip.htm
- Eastwood, B. (2016). Hip arthroscopy. Medscape. Accessed January 11, 2017. http://emedicine.medscape.com/article/2500026-overview#a1
- Byrd, J.W.T. (2016). Hip arthroscopy. American Academy of Orthopedic Surgeons. Accessed January 11, 2017. http://orthoinfo.aaos.org/topic.cfm?topic=A00572
- Byrd, J.W.T. (2016). Femoracetabular impingement. American Academy of Orthopedic Surgeons. Accessed January 11, 2017. http://orthoinfo.aaos.org/topic.cfm?topic=A00571









 Provided below are documents to help with the process of the procedures including Pre-op outline, Pre-op letters to provide to primary care providers and an AUASS scoring sheet. Feel free to contact us with any other questions regarding orthopedic doctor resources.
Provided below are documents to help with the process of the procedures including Pre-op outline, Pre-op letters to provide to primary care providers and an AUASS scoring sheet. Feel free to contact us with any other questions regarding orthopedic doctor resources.